Eyelid dermatitis
- February 3, 2022
- by NATALIYA KUSHNIR
- Articles
What Is eyelid dermatitis?

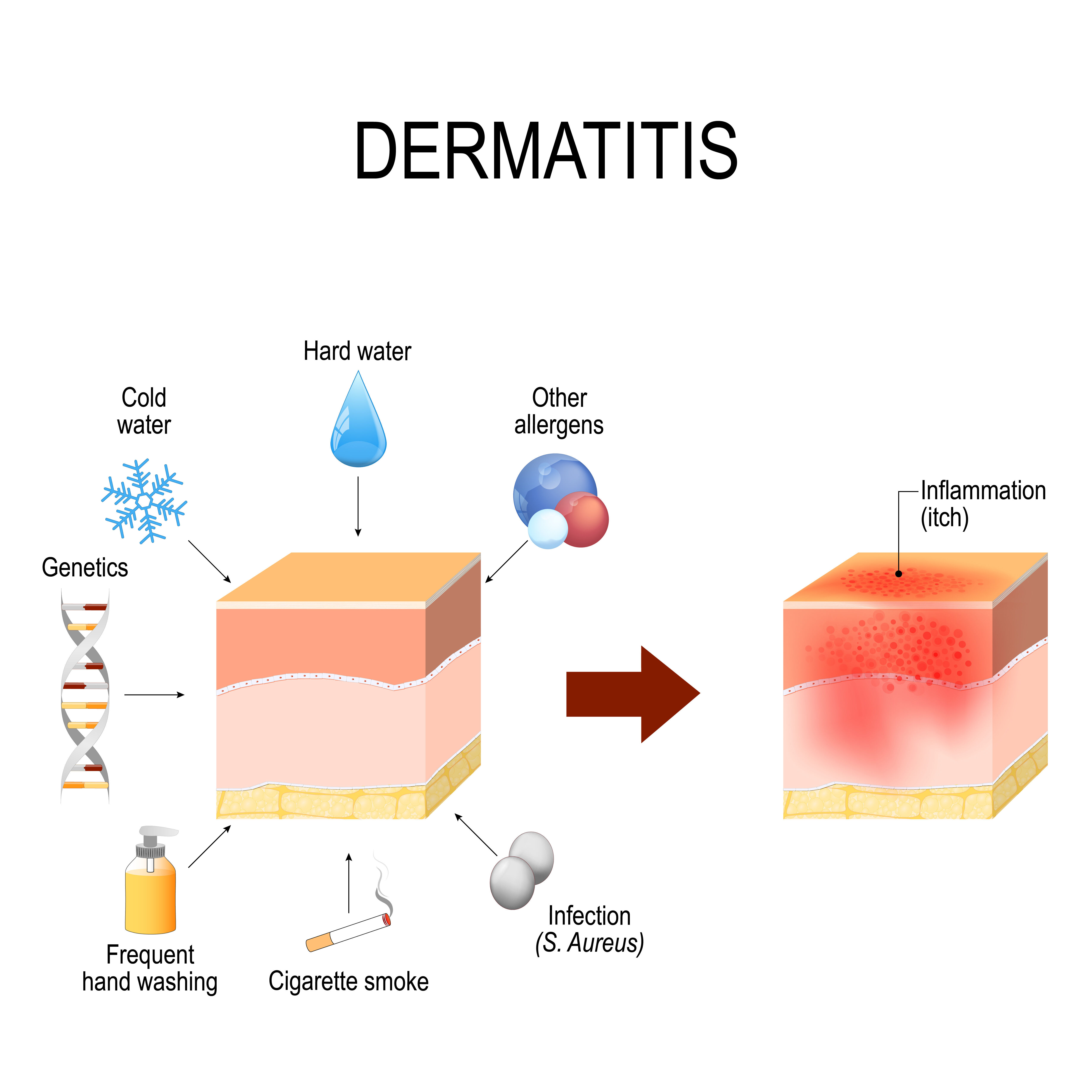
The inflammation of the eyelids is called a dermatitis in medicine. It comes from two roots – dermis – skin and –itis – inflammation. So, any process that causes an inflammatory reaction of the tissues of the eyelid will be classified with the same name. there are many types of the dermatitis, which we will describe in this article.
It is important to collect the whole history of your problem, which will help a doctor to identify the specific reason an inflammation of the eyelids. Why is that important? Because if the cause is identified correctly, you will receive treatment that will stop the process and you will feel healthy again.
Issues affecting the skin elsewhere on the body, such as atopic dermatitis, insect bites, cellulitis, and necrotizing fascitis, can occur on the skin of the eyelid. Methicillin-resistant Staphylococcus aureus (MRSA) colonization and infections can also affect the eyelid. Systemic processes, such as autoimmune disease, metastatic cancer, heart failure, and nephrotic syndrome, can manifest in the orbital region.
Whom do you need to see with eyelid dermatitis?

Well, that is an interesting question, as many specialists are involved in a treatment of eyelids. We recommend to start with a primary care. If the symptoms are sudden and unbearable – look for a doctor-on-call, an urgent care or even an emergency room. While you will receive an immediate treatment, the cause may not be determined. You will be likely referred to a specialist who treats eyelid dermatitis:
- Allergist
- Dermatologist
- Ophthalmologist
- Natural doctor
It is likely you will be scheduled for additional tests, especially if these problems are recurring (happening not once). Sometimes, if you know the problem is allergic, you can skip going to the primary care and just look for the nearest or best allergist around you.
Many of the situations with eyelid dermatitis are chronic with periods of getting better or worse. The longer you wait to get to the bottom of the problem, the more likely you will not be able to stop it easily. Why? Because it is easier to deal with inflammation before it got into a chronic form and got out of control.
Symptoms
Eyelid dermatitis symptoms are straightforward:
- Itching of the eyes (causing excessive rubbing)
- Swelling of the eyelids
- Eye discharge with crusting of the eyelashes
- Rash or redness of the eyelid skin
- Excessive tearing
- Pain or burning sensation
- Eyelashes falling out
Not all the symptoms may be present, based on the cause of the problem. These symptoms can all come at once (acute form) or appear and disappear in a timeline (chronic form).
Types and causes

Dependent on what caused eyelid dermatitis, there are specific diagnoses that doctor will come up with in your medical chart. Can a diagnosis change? Yes. Sometimes it is difficult to distinguish between different forms of dermatitis. So, there can be a “working” diagnosis that will change once the cause is found. Also, the same disease sometimes is called different names when an eye doctor sees it or an allergist diagnosed it. That happens because different specialties sometimes historically identify diseases or symptoms differently, and give it various scientific names.
Allergic contact dermatitis
Allergic contact dermatitis is when an allergy-causing substance came in direct contact with the body and triggered an allergic reaction. It can start any place on the body, so the eyelid dermatitis will be just a symptom of the systemic problem – not a separate disease.
Irritant contact dermatitis
Irritant contact dermatitis is caused by an abrasive chemical that got in a direct contact with skin, and managed to get through the upper protective layers of epidermis into dermal part where the immune cells acknowledged it as an intruder and attacked it. Once such reaction (sensitization) happened, each subsequent time the same chemical gets in a direct contact with the skin a massive immune reaction (involving white cells) starts.
Atopic dermatitis
Atopic dermatitis is regarded more as a part of systemic atopy – allergic condition of the immune system. More clinicians start seing that in order for skin to start reacting to an allergen, a bigger abnormal reaction of the immune happens first. It is a combination of the genetics (predisposition) and environmental factors that start the whole atopy. Then some people who genetically have weaker lungs will develop asthma, while others with a “chep skin” will develop atopic dermatitis. Patchy red itchy rash will first appear in certain locations on the baby, but later change the pattern in adult. Before doctors thought that it is two different conditions, but now it is recognized that the disease is the same only changing the location of inflammation as hormonal maturation happens.
Before scientist thought that atopic dermatitis was only affecting skin, when now numerous literature reports have long confirmed the relationship between the disorder and a growing number of ophthalmic manifestations such as keratoconus and retinal detachment (for example).
Seborrheic dermatitis
Seborrheic dermatitis is a common skin condition in infants, adolescents, and adults. The characteristic symptoms-scaling, erythema, and itching-occur most often on the scalp, face, chest, back, axilla, and groin. Seborrheic dermatitis is a clinical diagnosis based on the location and appearance of the lesions. The skin changes are thought to result from an inflammatory response to a common skin organism, Malassezia yeast.
Diagnosis
In order to make a correct diagnosis, a doctor needs to rule out other problems. Here are some inflammatory eyelid conditions:
| Blepharitis | Inflammation of the base of the eyelashes and/or distal aspects of the eyelids; inflammation of the lacrimal gland | Irritated lid edges or eyelash |
| Chalazion | Noninfectious obstruction of meibomian tear gland | Discrete mass within the lid present for two or more weeks |
| Dacryoadenitis | Inflammation of the lacrimal gland | Circumscribed tender mass in upper outer lid; if advanced, may appear as the diffuse inflammation of preseptal cellulitis |
| Dacryocystitis | Inflammation of the lacrimal sac and duct | Tender mass at the medial aspect of the lower eyelid; if advanced, may appear as the diffuse inflammation of preseptal cellulitis |
| Hordeolum or stye | Hordeolum: infection of the meibomian (sebaceous) glands | Papule or furuncle at distal lid margin |
| Stye: infection of the sweat gland (gland of Zeis) of the eyelid | ||
| Orbital cellulitis | Infection of the soft tissues within the orbit, posterior to the orbital septum, often due to spread from local sinus disease | Red, swollen, tender eyelid; extraocular movements limited because of pain or muscle edema; vision changes, diplopia; in children, fever and ill appearance |
| Preseptal cellulitis | Infection of lid tissues around the orbit, often with local skin defect | Red, swollen, tender eyelid; full extraocular movements; no vision changes |
After clinical diagnosis was assumed, certain tests will help determine the cause.
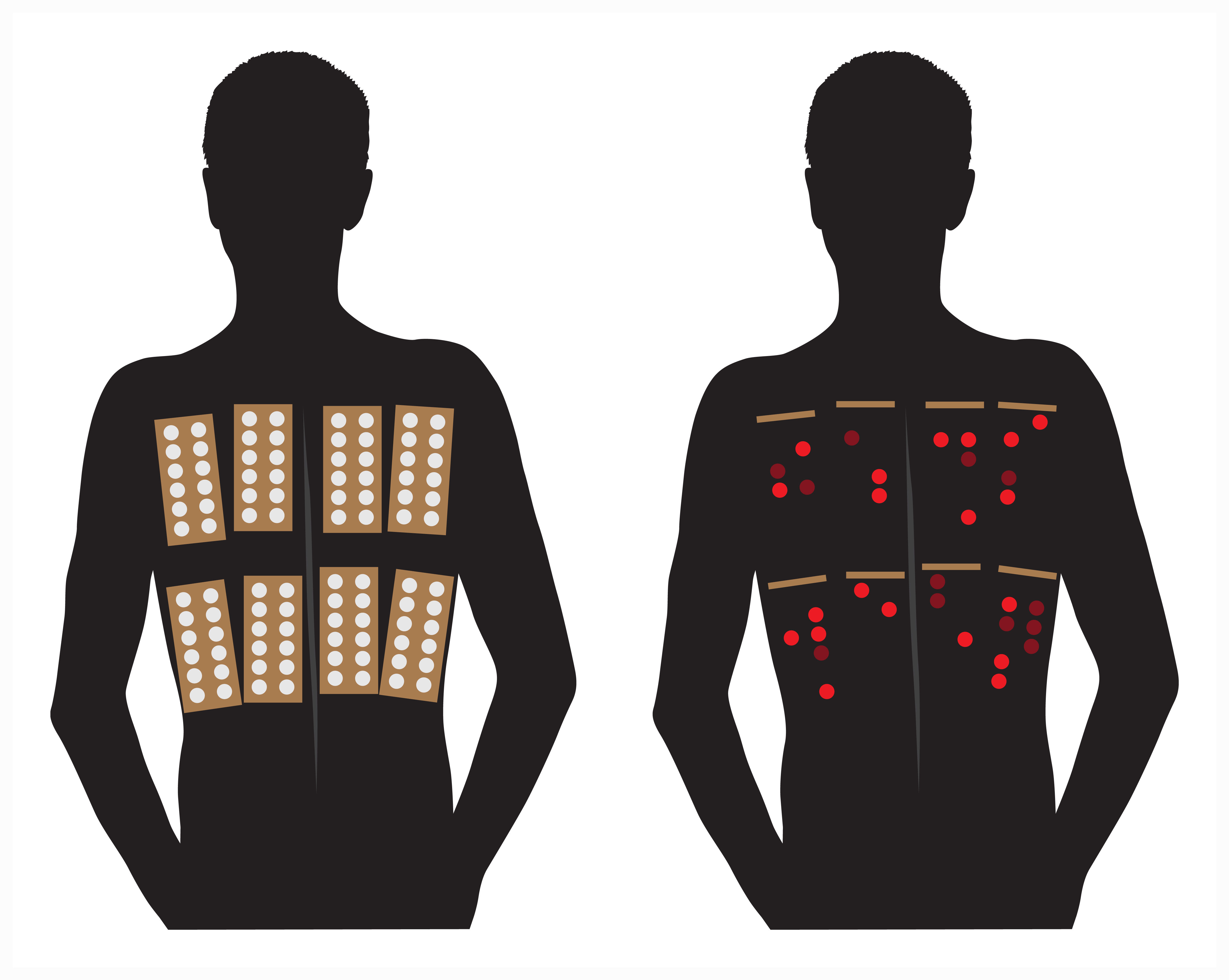
Patch test. This test is used to determine contact dermatitis. A number of known chemicals are made into small patches that can be placed on the skin for 24 hours. The results (skin reaction similar to the rash that happens) are checked by the nurse for immediate reaction (when the test is removed), and then for delayed reaction (at 48 and 72 hours). There are certain testers that are commercially available, while almost all suspicions chemicals from your household can be custom-made into tests. This is a tedious test, but when you cannot figure out what is causing irritant dermatitis – it’s a saver!
Skin prick (scratch) test. It is also known as allergy skin test. This is a sure and fast way to find out if you have an environmental or food allergy. Each protein in question is applied on the skin with the tiny device – a prick. It delivers the allergen right under the epidermal layer where it is easily recognized by the immune cells if the allergy exists. A small itchy red bump is formed almost immediately – that is what a nurse will look for and measure. A positive test is counted if the reaction measures more then 3 mm. this test is done in the allergist’s office, and takes 30 min. you will receive the test results which will tell you for sure which allergens to avoid, and if you can ask for Sublingual drops or allergy shots as a treatment.
Intradermal allergy test. In certain cases an allergist may decide to check an intradermal allergy test – this is a deeper injection of the allergen into the dermal skin layer. It is done with the tiny syringe – same that is used for insulin injections. Why is it needed? If there is a strong suspicion for a certain allergen being responcible for the symptoms, but the skin prick was negative, sometimes the cells that cause reaction may be sitting deeper in skin. Then an intradermal test will show if there is a true allergy. Such test is used with caution, as the systemic allergic reactions are more common. Intradermal test is also used as a single possible test in a Hymenoptera allergy (bee allergy, wasp allergy, yellow jacket allergy etc.)
Radioallergosorbent test. This is a laboratory blood test for allergy. A small amount of blood that may contain immune antibodies to a certain allergen is mixed with a series of components, the end-point is emission that is measured from a mixture that contains antibodies – it is measured and reported in units. This test is not perfect – if the amount of antibodies in the blood is very high, then non-specific binding will cause false positive reaction (meaning telling you that you have allergy to something that in reality is not). At the sam time people who have very small amount of antibodies will have false negative result – their true allergens will not show up because of the threshold of the detection. This test is used as a screening, or if someone cannot be tested by skin test.
Complications
The most frequent and potentially serious problem is infection. Due to chronic inflammation the barrier of the skin is open and the normal bacteria that usually happily lives on the skin can get inside. That can cause immediate spread. Also, the resistance to antibiotics is a serious problem, as AD is a recurrent problem, so using antibacterial creams often can cause these bacteria to become resistant (like MRSA).

Eye involvement is also a complication that can lead to blindness – do not wait long if a child is complaining of severe eye pain, or cannot open an eye. you need to see an ophthalmologist right away.
If an eyelid dermatitis is going on for a while, you may see eyelashes and eyebrows falling out. Also, the glands that produce the oily lubricant for the eye may get clogged. This can lead to a dry eye syndrome, or a dysfunction of the glands – stye and chalazion.
Treatment
Red swollen eyelid is one of the most common conditions seen in the primary care, so there are certain guidelines that were developed:
- Immediate imaging of the orbits and ophthalmology consultation are warranted for patients presenting acutely with vision changes, decreased extraocular movements, or penetrating trauma.
- Patients with herpes zoster ophthalmicus should be treated promptly with antiviral medication to avoid adverse outcomes to the cornea and to the patient’s vision.
- In patients with preseptal or orbital cellulitis, clinicians may consider empiric antibiotic coverage for methicillin-resistant Staphylococcus aureus, depending on local bacterial prevalence.

Moisturize. The skin that is dry becomes itchy and cracked, which invites the rest of the inflammation. Emolyents were found very effective in preventing the eczema and AD. Do not use OTC creams and moisturizers – you need to ask a doctor about true dermatology-recommended creams that are usually offered in medical offices. You can try samples and then order the cream that works the best. Creams with ceramide are the best in helping with the AD.

Remember – the eye is very sensitive to anything that gets inside. Be very careful in applying creams around your child’s eye – if the cream gets inside and burns the child will immediately start crying and rubbing eyes, which will lead to more of the cream getting in. it is best to use natural oils, such as avocado or olive oil to moisturize child’s eyelids lightly at night.

Emollients (e.g. glycol and glyceryl stearate, soy sterols) lubricate and soften the skin, occlusive agents (e.g. petrolatum, dimethicone, mineral oil) form a layer to retard evaporation of water, while humectants (e.g. glycerol, lactic acid, urea) attract and hold water.
Use calcineurin inhibitors
Two TCIs are available, topical tacrolimus ointment (0.03% and 0.1% strengths) and pimecrolimus cream (1% strength). Both agents have been shown to be more effective than vehicle in short-term (3 to 12 weeks) and long-term (up to 12 months) studies in adults and children with active disease.
Use corticosteroids
Topical corticosteroids are recommended for AD-affected individuals who have failed to respond to good skin care and regular use of emollients alone.
A variety of factors should be considered when choosing a particular topical corticosteroid for the treatment of AD, including patient age, areas of the body to which the medication will be applied, and other patient factors such as degree of xerosis, patient preference, and cost of medication.
Twice daily application of corticosteroids is generally recommended for the treatment of AD; however, evidence suggests that once daily application of some corticosteroids may be sufficient.
Proactive, intermittent use of topical corticosteroids as maintenance therapy (1–2 times per week) on areas that commonly flare is recommended to help prevent relapses and is more effective than use of emollients alone.
The potential for both topical and systemic side effects, including possible hypothalamic-pituitary-adrenal (HPA) axis suppression, should be considered, particularly in children with AD in whom corticosteroids are used.
Monitoring by physical examination for cutaneous side effects during long-term, potent steroid use is recommended.
No specific monitoring for systemic side effects is routinely recommended for patients with atopic dermatitis.
Patient fears of side effects associated with the use of topical corticosteroids for AD should be recognized and addressed to improve adherence and avoid under-treatment.
Prevention

As with all atopic and inflammatory diseases – we give recommendation to keep the whole body healthy:
- Use as few chemicals in your environment as possible
- Do not use antibacterial fragrant soaps and shampoos
- Use water filtration whenever possible
- Use emolyents (preferably natural or hypoallergentic) after the bath or shower to preserve moisture in the skin
- Use hypoallergenic detergents and soaps that are recommended for babies on everything that touches the baby skin
- Take probiotics and fish oil daily
- Eat organic balanced meals
After all, the skin is one of the largest organs of the body which reflects all your health, and protects you from all outside dangers – take a good care of it.
